8 Zoonotic Diseases Shared Between Animals and Humans
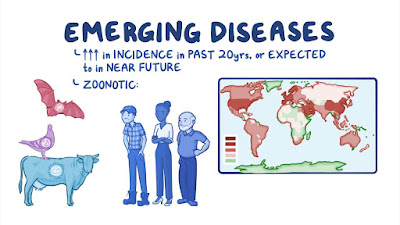
A zoonosis is an infectious disease that has jumped from a non-human animal to humans. Zoonotic pathogens may be bacterial, viral or parasitic, or may involve unconventional agents and can spread to humans through direct contact or through food, water or the environment.
8 Most Common Zoonotic diseases and their prevention
A. Diseases that are transmitted between animals and humans
There are 120 known Zoonoses agents according to CDC.
Risk of contracting disease varies depending on the disease and Situation
B. Focus on farming
Working on farms increase risks — why?
Shared space and shared air with many animals.
Increased contact with animals.
Animals may appear to be healthy but carry infectious diseases.
What kinds of animals transmit Zoonoses?
Cattle, Swine, Goats, Cats, Dogs, Ticks, Squirrels, Raccoons
And Other wild animals.
How are diseases transmitted?
Every day contact.
Transporting carcasses and By-products
Scratches or bites
From milk and from milking
Contaminated soil
Contaminated meats.
C. What are the common Zoonotic Diseases?
1. Campylobacter
Common carriers: Cattle, Sheep, Pigs, Dogs, Rodents and Poultry.
Transmission: Direct contact with contaminated food Contaminated animals
Clinical Presentation: Stomach ache, nausea, headache, diarrhea.
2. Salmonellosis
Common carriers: Cattle, Cats, Dogs, Horses, and Poultry.
Transmission : Direct contact with animal or feces, Food contamination from infected animals
Clinical presentation: Chills, fever, headache, diarrhea and vomiting.
3. Encephalitis
Common Carriers: Horses and Rodents
Transmission : Mosquito bite, tick bites.
Clinical presentation: Lethargy, fever, headache, and disorientation.
4. Rabies
Common Sources: Cats, dogs, raccoons, bats, foxes and skunks.
Transmission : Animal bites, contact with infected tissue, fluid and
Feces.
Clinical Presentation: Fever, headache, confusion, seizures, excessive
Salivation and death.
5. Psittacosis
Common carriers: Pigeons, parrots, turkeys, and parakeets.
Transmission : Inhalation from infected birds, carcasses,
secretions, and contaminated facilities.
Clinical Presentation: Fever, headache, and pneumonia.
6. Ringworm
Common carriers: Cattle and Cats
Transmission : Direct contact
Clinical Presentation: Skin lesions
7. Toxoplasmosis
Common carriers: Cats, sheep and undercooked meat.
Transmission : Ingestion of infected meat, fecal contaminated soil.
Clinical Presentation: Fever, swollen lymph nodes. Abortion, still-birth.
8. Scabies
Common carriers: Dogs, and Raccoons
Transmission : Direct contact with infected animals
Clinical Presentation: Itching skin lesions.
Prevention and Control
1. Use an uncontaminated water supply.
Many diseases are carried in animal wastes that leak into water supplies
Make sure wells are properly constructed to avoid contamination
from livestock, animal and human wastes.
Add Chlorination to water.
Follow instruction for appropriate disposal of wastes.
2. Prevent food contamination
Avoid unpasteurized milk. Wash hands and clean and disinfect
kitchen surfaces before, during and after handling food.
Wash raw fruits and vegetables.
Cook food immediately after defrosting.
Cook all poultry to an internal temperature of 180 degrees, and
ground beef to an internal temperature of 160 degrees.
Refrigerate leftovers immediately.
3. Avoid contact with diseased animals and prevent pets from contact with Rodents and wild animals.
(e.g. Ticks carried by pets can cause Lyme
disease or Rocky Mountain Spotted Fever. Raccoons, foxes
and other mammals can transmit rabies.) Protect pets from getting and transmitting disease.
Vaccinate cats and dogs against rabies
Do not keep wild animals as pets.
4. Prevent Tick Bites
Wear appropriate clothing.
Use Tick repellent
5. Treat animal scratches and bites seriously
Wash the area with soap and water
Apply anti-bacterial medication
Major Zoonotic diseases in Kerala
Anthrax
It is a zoonotic illness caused by Bacillus anthracis. Sporadic cases continue to be reported from many parts of the India. anthrax meningo-encephalitis (AME) are also becoming common in patients infected with Anthrax. Most cases seem to occur in labourers who gave history of handling animal meat or skin of infected animals. In a few instances `insect bite’ has been attributed. The meningo-encephalitic form of the disease has a very bad prognosis. Patients with this form of disease died inspite of treatment with high dose penicillin. The typical bacilli are easily seen in the CSF in AME cases and is diagnostic of the condition. The cutaneous form of illness has a benign course and responds favourably to penicillin treatment. The disease needs to be prevented with proper legislation for meat handling as well as effective immunisation of animals. (Indian Journal of Medical Microbiology. 1996 Apr; 14(2): 63-72 )
The clinical presentation is so characteristic that the diagnosis is rarely missed by physicians familiar with the disease. The exposed part of the skin begins to itch and there is a papule at the inoculation site. The papule becomes a vesicle and then a depressed, black, non-painful eschar 1-3 cm diameter that leaves a permanent scar. There may be surrounding edema and draining lymph nodes may become enlarged. If untreated, septicemia and death can occur in 5-20% of cases. If treated, fatalities are extremely rare.
How disease transmitted in human?Animals dying of anthrax produce enormous quantities of bacteria in their tissues. If the carcass is opened, the bacilli sporulate, contaminating the environment. Contaminated soil, contaminated animal products (including hides, fur, food), or environmental contamination by spores are also sources of the bacteria. The bacterial spores prefer alkaline environments (pH > 6) with abundant organic material, but can survive almost anywhere. Human to human transmission is extremely rare, even with pulmonary disease.
Leptospirosis
[Weil’s disease, Hemorrhagic jaundice (Leptospira icterohaemorrhagiae), canicola fever (L. canicola)
AGENT: Spirochete, Leptospira. Pathogenic leptospires belong to the species Leptospira interrogans
RESERVOIR AND INCIDENCE
Rats, mice, field moles, guinea pigs, gerbils, squirrels, rabbits, hamsters, reptiles, nonhuman primates, livestock, and dogs. *Rodents are the only major animal species that can shed leptospires throughout their life-span without clinical manifestations. Active shedding by lab animals can go unrecognized until personnel handling the animals become clinically ill.
TRANSMISSION: Handling affected animals, contaminating hands, or abrasions with urine, or aerosol exposure during cage cleaning are most common. The organism is often transmitted to humans by the urine of the reservoir host. The organism may also enter through minor skin lesions and probably via the conjunctiva. Many infections have followed bathing or swimming in infected waters.
DISEASE IN HUMAN: Ranges from inapparent infection to severe infection and death. Biphasic Illness a. Weakness, headache, myalgia, malaise, chills, & fever. b. Leukocytosis, painful orchitis (testes not usually enlarged), conjunctival effusion, and rash. Icteric leptospirosis (Weil’s syndrome-usually caused by L. icterohaemorrhagiae) is the most severe form of the disease, characterized by impaired renal and hepatic function, abnormal mental status, hypotension, and a 5-10% mortality rate. Signs and symptoms are continuous and not biphasic.
DIAGNOSIS: Early in the disease, the organism may be identified by darkfield examination of the patient’s blood or by culture on a semisolid medium. Culture is difficult and requires several weeks. A rapid diagnosis is made with the DOT-ELISA test.
TREATMENT: Penicillins or tetracyclines.
PREVENTION\CONTROL:Vaccination in cattle, swine, and dogs Avoid swimming in or drinking from potentially contaminated water. Protect workers by providing boots and gloves. Rodent control. Drain wet ground. Doxycycline chemoprophylaxis for persons at high exposure.